Chapter Five
ASC Accreditation and Compliance Issues

Accreditation and compliance are vital aspects of ASC management, requiring continuous attention and structured processes. Earning and maintaining accreditation demonstrates an ASC’s commitment to patient and staff safety, high-quality care, and operational excellence. Accreditation not only enhances reputation among patients, physicians, and payers, but also strengthens compliance with state and federal requirements.
Maintaining Compliance
Although ASC accreditation isn’t mandated federally, many states and private payers require it for licensing or contracting. Maintaining accreditation takes continuous attention and disciplined processes. The following best practices can help your ASC prepare for surveys and sustain compliance year-round.
1. Keep accreditation in focus
Make accreditation part of your culture.
- Discuss requirements regularly in staff meetings.
- Highlight relevant standards in internal communications.
- Share best practices and success stories from other ASCs.
Frequent reminders reinforce that compliance is everyone’s responsibility—not just a task during survey season.
2. Conduct mock surveys
Simulated surveys help identify and correct weaknesses before regulators find them.
- Designate an internal lead or hire an external consultant familiar with your accrediting body’s standards.
- Have mock surveyors observe daily practices, review records, and interview staff.
- Debrief after each mock survey, documenting corrective actions and next steps.
Proactive preparation reduces stress and ensures your team stays audit-ready.
3. Invest in resources that support compliance
Compliance thrives when staff have the right tools and education.
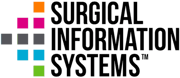
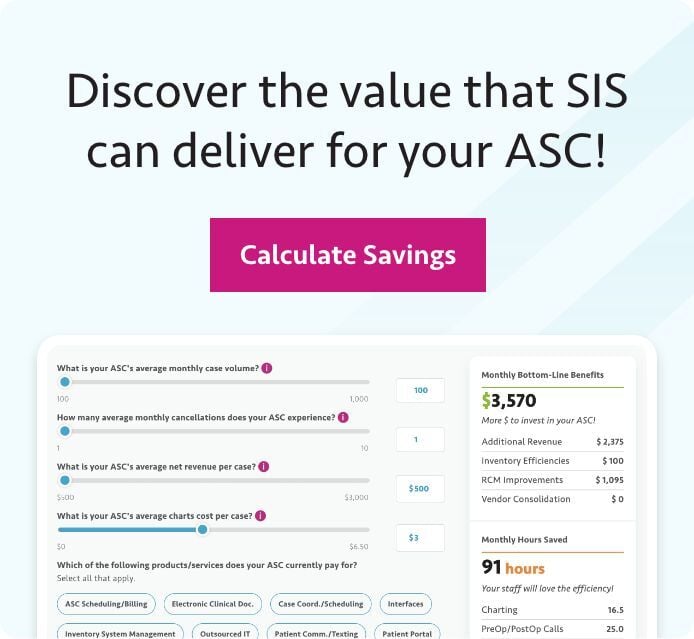
- Use ASC-specific documentation and analytics software to improve accuracy and reporting.
- Send team members to ASC conferences, webinars, or industry events.
- Encourage subscriptions to professional publications covering accreditation updates.
Empowered, informed employees are your strongest compliance asset.
4. Adopt an ASC-specific electronic health record (EHR)
An ASC-tailored EHR simplifies charting, documentation, and survey readiness. Choose a vendor that keeps systems current with CMS and accrediting body standards so your ASC can easily produce consistent, compliant records during inspections.
5. Perform regular regulatory compliance checks
Routine internal audits keep your ASC aligned with CMS, OSHA, CDC, NFPA, CLIA, and state requirements. Delegate checks by frequency:
Daily: Medication refrigerators, blanket/fluid warmers, crash cart, malignant hyperthermia (MH) cart, emergency equipment, exits and corridors are clear, autoclaves
Weekly: Eyewash stations, emergency generator, nurse call system
Monthly: Exit light inspection, emergency lighting, generator, expired medications, Fire extinguishers, crash cart (interior contents), pest control
Quarterly: Complete notes, reports, and minutes from QAPI committee (including information from safety, infection prevention, pharmacy coordinators, and review occurrence reports and peer review); fire drills; clean the ice machine; send dosimeters for readings; check the HVAC
Annually: Review/revise safety plan; summarize fire extinguisher checks and check fire alarm system, including smoke and fire dampers; disaster drill; medical gas and vacuum system inspection; review and revision of policies and procedures; DEA narcotic count; staff immunizations; training (HIPAA, OSHA, emergency management plan); contract quality review; fire door inspection; HVAC duct cleaning; C-arm/laser inspections; radiation safety checks
At least annually: Check personnel records for date-sensitive information, competencies, credentialing and recredentialing, peer review, mandatory state reports and CMS quality indicators
Assign responsibilities to managers, track completion, and hold teams accountable. Outsourcing some checks can reduce internal workload without sacrificing compliance quality.
Achieving QAPI Objectives
An effective Quality Assurance and Performance Improvement (QAPI) program demonstrates a commitment to continuous improvement, and it’s critical for CMS compliance. Weak QAPI programs can jeopardize accreditation and cause missed opportunities for operational gains.
Here are some areas of focus to help you maximize the benefits of QAPI while meeting regulatory requirements:
1. Collect and analyze data
Identify trends and opportunities using existing ASC data sources—financial reports, patient and staff satisfaction surveys, and incident logs. Let this data guide your study topics.
2. Focus on impactful improvements
Select only a few QAPI studies each year, but make them count. Engage staff in identifying focus areas, especially those that affect patient safety, satisfaction, or workflow efficiency. Involving your team drives ownership and successful implementation.
3. Plan and execute studies methodically
Create a QAPI calendar detailing when topics are chosen, studies are conducted, and results reviewed. Regular committee meetings ensure progress and accountability.
4. Continuously review program performance
Evaluate your quality initiatives regularly. Track progress, review in-progress studies, and identify new areas for review based on feedback, surveys, or new regulations.
5. Learn strategically from others
Benchmarking other ASCs can inspire useful study topics, but avoid copying. Tailor projects to your data, resources, and staff expertise to ensure relevance and results.
6. Avoid common QAPI pitfalls
Watch out for these missteps that undermine program effectiveness:
- Choosing topics with limited potential impact
- Pursuing outdated or irrelevant issues
- Confusing ongoing monitoring with limited-time performance studies
- Not concluding with actionable improvements
- Starting but not completing studies
- Copying topics from other ASCs without relevance to your own facility
The Bottom Line: Building a Culture of Continuous Compliance
Accreditation is not a one-time event. It’s an ongoing commitment to quality, safety, and accountability. By embedding compliance into daily operations, investing in staff education and technology, and maintaining a proactive QAPI program, your ASC can stay survey-ready, strengthen patient trust, and ensure long-term success.
Back to Top
 What's Next for the ASC Industry? SIS and industry experts discuss current challenges and future opportunities for ASCs, providing actionable recommendations and best practices to drive growth, efficiency, and quality outcomes.
What's Next for the ASC Industry? SIS and industry experts discuss current challenges and future opportunities for ASCs, providing actionable recommendations and best practices to drive growth, efficiency, and quality outcomes.