Chapter One
Building the Foundation for Successful ASC Billing Operations

Ambulatory surgery centers operate in a dynamic and highly regulated billing environment. If ASCs aren’t current on evolving compliance and billing requirements and best practices for accurate coding, they may face challenges like lost revenue, increased claims denials, and decreased patient and physician satisfaction.
The good news is that ASCs can take a proactive approach to billing that maintains financial health and keeps operations running smoothly.
Establishing a Solid Billing Framework
Every ASC, whether managing billing internally or through a strategic partner, must prioritize building a foundation rooted in current industry knowledge, streamlined coding workflows, and proven compliance practices. This foundation is essential for maintaining financial health, minimizing risk, and supporting exceptional patient experiences.
Mastering Industry Guidelines for Compliance
A comprehensive understanding of both federal and private (commercial) payer requirements serves as the first step toward billing excellence. While Medicare policies provide clear guidance, private payers often implement distinct rules regarding coding, modifiers, authorization, and documentation requirements. Successfully navigating these differences is critical to avoiding costly errors and protecting revenue.
Compliance is not a one-time event but an ongoing commitment that needs discipline. It requires:
- Continuous staff education to maintain expertise
- Diligent monitoring of regulatory updates, including CMS (Centers for Medicare & Medicaid Compliance) quarterly changes
- Implementing regular internal audits to identify and address areas for improvement
Examples of areas ASC administrators should pay particular attention to are proper modifier usage and multi-procedure discounting, as these often result in claims denials, collections delays, and reduced reimbursements.
It is essential to recognize that payer policies tend to differ significantly from CMS guidelines. Many insurers impose specific documentation requirements for implants, bundled services, and unlisted codes. Understanding these distinctions is fundamental to protecting revenue and maintaining compliance.
👉 Related reading: Ambulatory Surgical Billing: Guidelines, Rules, and Requirements
Precision in ASC Coding: The Key to Optimal Performance
Correct coding is the cornerstone of a healthy revenue cycle. ASC coding demands an expert grasp of CPT, HCPCS, ICD-10, and payment indicators unique to surgical facilities. Staff must be vigilant in closing documentation gaps, correctly assigning the appropriate modifiers, and sequencing codes — especially in multi-specialty centers where navigating complex and highly varied cases is the norm.
Common challenges also include mismatches between operative notes and CPT codes, outdated fee schedules, and device-intensive procedure errors. Nuanced issues, such as bilateral procedures, reporting implantable devices, and identifying separately billable services, require specialized expertise. To address these needs, many ASCs benefit from working with dedicated coding professionals who can reduce claim errors and accelerate reimbursement.
Independently owned ASCs and those managing their revenue cycle in-house can overcome coding challenges by taking proactive steps to strengthen their processes. Regularly reviewing coding workflows and ensuring internal policies align with current CMS and payer guidelines is a great place to start. Establishing a routine for updating fee schedules, validating CPT code assignments, and clearly documenting services in medical records can go a long way in minimizing discrepancies. Additionally, tapping into educational resources and conducting periodic coding audits can empower your team to stay up-to-date and catch potential issues early, ensuring smoother claim submissions and better outcomes.
👉 Related reading: Understanding ASC Coding to Achieve Faster and More Accurate Billing
Addressing Denials and Enhancing Revenue Integrity
Errors in coding or compliance create far-reaching effects, resulting in claim rejections, reimbursement delays and loss, and increased administrative burden. These issues can negatively impact patient satisfaction and disrupt overall cash flow, while the cost and time required to rework denied claims can further reduce operational efficiency.
Proactive steps ASC administrators and billing professionals can take to address denials head on include:
- Investing in robust staff training to maintain coding expertise
- Enforcing detailed documentation standards for each specialty and procedure your ASC performs
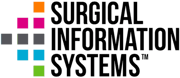
- Utilizing advanced technology solutions to identify errors before submitting claims
Leadership can also analyze denial trends, such as authorization issues or incorrect modifier usage, and create targeted improvements to reduce recurring problems.
Accuracy and Compliance: Pillars of Financial Success
While operational efficiency is important, long-term revenue stability depends on consistent accuracy and regulatory compliance. When these elements are closely aligned, ASCs benefit from:
- Faster claims processing for accelerated payments
- Reduced risk and more predictable financial forecasts
- Stronger foundation of trust with payers
Partnering with an organization specializing in ASC billing and coding can bring significant value. Expert teams can identify trends, recommend workflow enhancements, and help resolve even the most complex billing challenges. Whether you’re developing new billing processes or refining established operations, focusing on compliance and precise coding is essential to building a resilient, successful ASC.
In addition, by establishing a strong foundation and prioritizing compliance, your ASC can achieve efficient operations, financial stability, and the delivery of exceptional patient care. The investment in proper billing foundations can pay dividends through improved cash flow, reduced administrative workload, and enhanced operational performance.
Back to Top
 What's Next for the ASC Industry? SIS and industry experts discuss current challenges and future opportunities for ASCs, providing actionable recommendations and best practices to drive growth, efficiency, and quality outcomes.
What's Next for the ASC Industry? SIS and industry experts discuss current challenges and future opportunities for ASCs, providing actionable recommendations and best practices to drive growth, efficiency, and quality outcomes.